I don't always pay attention... Without looking into details, and peripheral exposure, I thought the Big Blue Test was just a way to get more people to test their blood sugar. I know there are a few people with diabetes out there who are in denial and don't test their blood sugar, it might help them snap out of it and get more pro-active... but, when I realized that it was an "effects of exercise" experiment I became much more interested. I do this everyday and since I use a CGM I am seeing the impact immediately. It's no small thing. I'd encourage you to do it if you haven't.
When I take a brisk 20 minute walk I will usually see my insulin sensitivity kick in and my blood sugar will normally drop 30-40 points. It can make a correction work about 3x faster. For me, it's great to take a walk in the morning, and I don't have to bolus for my protein breakfast. I also take our dog for a walk after dinner and keep my post-dinner numbers in check.
Thursday, November 8, 2012
Friday, October 26, 2012
Health Data from October Blood Panel
I didn't receive any info from the lab before I saw my doctor, so I went in eager to see my numbers, just like the "good old days".
Thyroid
The measurement that was unresolved last time was my thyroid levels. I had a TSH of 5.5. My doctor wanted to let it ride and see what it would do over time. This time it was 5.62, which is a tad higher. This time we also tested my free T4, which is the actual thyroid hormone produced by the thyroid gland, and it showed to be 1.1, which is in the normal range. So does that mean that everything is normal? I don't know. Reverse T3 is sometimes the real problem indicator for type 1 diabetics, but that wasn't tested. My doctor is satisfied with the results. Since I haven't had any complaints about my energy levels for the past few months, I guess I'm satisfied too.
Thyroid & Lipids
I brought up the connection between lipids and thyroid and he said that it is more of a story if the thyroid is really out of whack. He said since I don't have any signs of CHD, he's not going to try to figure out my borderline lipids via thyroid tweaks. I agree with that. The markers are fuzzy, and it's made even more murky because of the medical establishment's tendency to get everyone on a pharmaceutical when lifestyle solutions might be safer.
So, yes... lipids.
Total cholesterol: 250
HDL: 72
Triglycerides: 56
LDL: 167
CHOL/HDLC ratio: 3.5
NON-HDL Cholesterol: 178
The non-HDL Cholesterol was one I hadn't seen before. The target range is listed as 30 mg/dL higher than the LDL cholesterol target. Perhaps this measurement takes into account the fact that LDL isn't actually measured, but rather calculated... and it's, sometimes incorrectly, assumed that you have a certain number of lipoproteins, regardless of size. I'll have to find out more about this measurement and target.
Glucose Control
My A1c was 6.4, which goes along with what my average sensor numbers have indicated. Right now I'm hanging out in the 6.1-6.4 "higher risk of diabetes" range. I'd love to get into the "decreased risk of diabetes" range at <5.7, but based on my efforts I don't know if that's ever going to happen. Plus, I am positive that I already have diabetes.
My blood glucose at the time of test was 79 mg/dL. I tested on my meter before and after my blood draw and got readings of 79 and then 85, and my sensor was reading 80. I guess everything was pretty accurate at that point in time. Good to know...
To be honest, I think i have settled into a routine with glucose control and it hasn't been too variable over the last 6 months. I wish I had more to report, but things are getting pretty quiet and I'm not really experimenting too much. Sometimes it's hard to know what to blog about because most days are pretty simliar.
I've been geeking out on looking at data across time lately, and I think I'll make some graphs that show trends throughout the past year.
Vitamin D
I made an effort to get daily doses of sun this summer, and I'm currently supplementing with liquid D3. I asked to have my levels checked and make sure I was on the right track. My levels were measured at 74 ng/mL. So, I'm in the top third of that range. My doctor said he's never seen anyone measure over the 100 ng/mL upper limit.
More Doctors...
I was planning to ask my doctor (an internist) for a referral to an endocrinologist. I thought maybe I'd get more aggressive treatment and relevant testing. I've started to realize that m doctor will probably go along with any additional tests that I feel are necessary, and he's always advocated for any devices that my insurance will cover. My long term relationship with him is good and we have mutual respect for each other. I feel pretty lucky to have him as my doctor. I decided to ask for a referral to a podiatrist for my plantar fasciitis, but held off on the endo request.
Thyroid
The measurement that was unresolved last time was my thyroid levels. I had a TSH of 5.5. My doctor wanted to let it ride and see what it would do over time. This time it was 5.62, which is a tad higher. This time we also tested my free T4, which is the actual thyroid hormone produced by the thyroid gland, and it showed to be 1.1, which is in the normal range. So does that mean that everything is normal? I don't know. Reverse T3 is sometimes the real problem indicator for type 1 diabetics, but that wasn't tested. My doctor is satisfied with the results. Since I haven't had any complaints about my energy levels for the past few months, I guess I'm satisfied too.
Thyroid & Lipids
I brought up the connection between lipids and thyroid and he said that it is more of a story if the thyroid is really out of whack. He said since I don't have any signs of CHD, he's not going to try to figure out my borderline lipids via thyroid tweaks. I agree with that. The markers are fuzzy, and it's made even more murky because of the medical establishment's tendency to get everyone on a pharmaceutical when lifestyle solutions might be safer.
So, yes... lipids.
Total cholesterol: 250
HDL: 72
Triglycerides: 56
LDL: 167
CHOL/HDLC ratio: 3.5
NON-HDL Cholesterol: 178
The non-HDL Cholesterol was one I hadn't seen before. The target range is listed as 30 mg/dL higher than the LDL cholesterol target. Perhaps this measurement takes into account the fact that LDL isn't actually measured, but rather calculated... and it's, sometimes incorrectly, assumed that you have a certain number of lipoproteins, regardless of size. I'll have to find out more about this measurement and target.
Glucose Control
My A1c was 6.4, which goes along with what my average sensor numbers have indicated. Right now I'm hanging out in the 6.1-6.4 "higher risk of diabetes" range. I'd love to get into the "decreased risk of diabetes" range at <5.7, but based on my efforts I don't know if that's ever going to happen. Plus, I am positive that I already have diabetes.
My blood glucose at the time of test was 79 mg/dL. I tested on my meter before and after my blood draw and got readings of 79 and then 85, and my sensor was reading 80. I guess everything was pretty accurate at that point in time. Good to know...
To be honest, I think i have settled into a routine with glucose control and it hasn't been too variable over the last 6 months. I wish I had more to report, but things are getting pretty quiet and I'm not really experimenting too much. Sometimes it's hard to know what to blog about because most days are pretty simliar.
I've been geeking out on looking at data across time lately, and I think I'll make some graphs that show trends throughout the past year.
Vitamin D
I made an effort to get daily doses of sun this summer, and I'm currently supplementing with liquid D3. I asked to have my levels checked and make sure I was on the right track. My levels were measured at 74 ng/mL. So, I'm in the top third of that range. My doctor said he's never seen anyone measure over the 100 ng/mL upper limit.
More Doctors...
I was planning to ask my doctor (an internist) for a referral to an endocrinologist. I thought maybe I'd get more aggressive treatment and relevant testing. I've started to realize that m doctor will probably go along with any additional tests that I feel are necessary, and he's always advocated for any devices that my insurance will cover. My long term relationship with him is good and we have mutual respect for each other. I feel pretty lucky to have him as my doctor. I decided to ask for a referral to a podiatrist for my plantar fasciitis, but held off on the endo request.
Thursday, October 25, 2012
Great post for T1 peeps, finally.
MarksDailyApple is one of my favorite blogs for diet and health topics, but I don't know if I remember Type 1 Diabetes ever being discussed as a main topic. Here it is.
I'm practicing many of the things that are mentioned as helpful for T1Ds. I think sleep is a factor that I didn't think mattered too much, but when I started sleeping the right amount, my insulin resistance really fell off.
Friday, October 19, 2012
Blood draw today!
I've been thinking I had a few things to write about, but, nothing earth shattering.
Immediately, I'm getting blood drawn today for my 6 month panel. My doctor is open to my suggestions and this time around I asked him for a more comprehensive tests for my thyroid levels. I've also asked for a Vitamin D metric so I will know if supplementation has been helpful. With the way things usually go, I'll have some results delivered to my phone by about Tuesday. In the meantime, I'm drinking black coffee, and it's kind of sad.
I have stopped doing at-home A1C tests every month because they went up in price ($26 test), I ran out of flexible spending funds, and my sensor data does tell me average blood glucose pretty accurately. That being said, when I stumbled across a great deal ($12 test) at a different drug store, I bought another kit. So, at the beginning of the month I ran the test and it was 6.7. I was coming off about two weeks of illness and some erratic glucose levels, so it was pretty much what I was expecting.
I've been learning a bit about how thyroid levels effect lipids, and for some people just treating the thyroid effectively brings the lipoprotein levels back to optimal. I'm not really concerned about my lipids, exactly, but they have been progressively going up, even while lifestyle has remained the same. The ratios are healthy, but the overal numbers are rising. It has happened in parallel with my suspicions that something is awry with thyroid function. I'd be curious whether my TSH levels are still clinically high, or whether the lipid levels have continued to change. When I mentioned this connection to my doctor he didn't seem to think it was a factor to worry too much about.
I recently heard Chris Masterjohn talk about cholesterol and he was mostly talking about the false perceptions about what were good signs and bad signs of cholesterol in the body. It was interesting that he recommended thyroid correction (even minute amounts) to fix most non-genetic problems with lipids.
I'll report back with more data. I'll be seeing my doctor about my blood work next week.
Immediately, I'm getting blood drawn today for my 6 month panel. My doctor is open to my suggestions and this time around I asked him for a more comprehensive tests for my thyroid levels. I've also asked for a Vitamin D metric so I will know if supplementation has been helpful. With the way things usually go, I'll have some results delivered to my phone by about Tuesday. In the meantime, I'm drinking black coffee, and it's kind of sad.
I have stopped doing at-home A1C tests every month because they went up in price ($26 test), I ran out of flexible spending funds, and my sensor data does tell me average blood glucose pretty accurately. That being said, when I stumbled across a great deal ($12 test) at a different drug store, I bought another kit. So, at the beginning of the month I ran the test and it was 6.7. I was coming off about two weeks of illness and some erratic glucose levels, so it was pretty much what I was expecting.
I've been learning a bit about how thyroid levels effect lipids, and for some people just treating the thyroid effectively brings the lipoprotein levels back to optimal. I'm not really concerned about my lipids, exactly, but they have been progressively going up, even while lifestyle has remained the same. The ratios are healthy, but the overal numbers are rising. It has happened in parallel with my suspicions that something is awry with thyroid function. I'd be curious whether my TSH levels are still clinically high, or whether the lipid levels have continued to change. When I mentioned this connection to my doctor he didn't seem to think it was a factor to worry too much about.
I recently heard Chris Masterjohn talk about cholesterol and he was mostly talking about the false perceptions about what were good signs and bad signs of cholesterol in the body. It was interesting that he recommended thyroid correction (even minute amounts) to fix most non-genetic problems with lipids.
I'll report back with more data. I'll be seeing my doctor about my blood work next week.
Monday, October 15, 2012
Yeah, I'm doing this...
 |
| I post pure text too often, so here's a personal photo. It's me. |
I've been a member of the GLU online community for a few months. It is specifically set up for Type 1 diabetics. I'm mostly active because I enjoy answering the polls they post each day. I use the iOS app and just open it up and answer the questions every day or two. It is pretty quick, but since I don't like typing much on my phone, I hardly ever add comments to the answers. However, I think it's pretty amazing to see 200+ people weigh-in on a topic. I'm going to comment further here.
Oct. 9th: Would you donate a blood sample for Type 1 diabetes research?
Yes.
I have never been part of a clinical trial, but I have gone through the arduous and worthwhile process of having my kids tested for auto-antibodies (they were negative!) through Diabetes TrialNet.
Oct. 10th: Do you celebrate your day of diagnosis?
No.
I do not.
Through my blog, I celebrate the fact that diabetes has had a profound impact on my character, and my approach to health and life. But, it's not a dia-versary or anything like that. I don't actually know the day that I was diagnosed. I know it was roughly 27 years ago in the late-summer of 1985.
Oct. 11th: Do you ever check the blood sugar of your friends and family?
Yes.
My kids sometimes ask me to test their blood sugar, and I sometimes do it.Yes.
Several months ago I tested everyone in my family's blood sugar at the same time. It was really interesting to see how much variation there is in the non-diabetic experience (85-142 mg/dl). Some really solid days I might even have tighter control than non-diabetics I know.
Oct. 12th: Have you ever had to deliver or receive a Glucagon injection?
No. I am happy about this. I have owned about 2 kits in my lifetime, and I currently have a non-expired one in my diabetic supplies cabinet. I'm not sure if anyone in my family or co-workers would be able to administer it. In my immediate family I have 3 diabetics, and I do not think any of us have ever needed injected glucagon. I have discussed this question myself...
Oct. 13th: What makes it challenging to be consistent when checking your BG or taking insulin?
Nothing. Since I use a pump and a CGM I have had much better focus on my blood sugar control. My CGM alerts me when I go up abruptly, and when I hit 150. Usually, this means that I don't get much above that. I eat low-carb, so the spikes are smaller and slower. It's easy to head off a rise before it gets too high. Before I was using a CGM it was easy for me to get busy teaching, during my work, day and forget to check blood sugar and bolus for meals. I think the CGM has made monitoring and correcting my glucose levels a natural part of my day.
Oct. 14th: If you wake up low in the middle of the night, do you ever wake somebody up so that they know?
No. My wife is a light sleeper and she is usually aware when I get up or leave the room. She doesn't always know why I wake up. Usually, a low will trip an alarm on my CGM. My wife is like the "princess and the pea" when it comes to CGM alerts. I wish they would wake me up, but in the end, she's the one that gets alerted. She often doesn't know what type of alert it is, she just wants some un-interrupted sleep!
Friday, October 5, 2012
Why did I never try this before?
I've been getting 6-7 days out of my Medtronic sensors, which are labeled to last three. When they time-out I just restart them and they keep working until the battery runs out, which is usually about the 7th day. By that time, I'm usually pretty grateful for the extra time and take it out and start a new one.
This week I had a particularly good one. It was comfortable, accurate, and I didn't want to see it go. When the battery ran out I disconnected the battery pack and recharged it. I started it up again and the sensor has continued to be accurate for another week, and I'm still using it on day 12. So, yes, with a battery recharge, the enzymes in the sensor have been able to keep working 4X longer than the stated life.
In my last blog post I was talking about the fact the box of expired sensors I was using were showing themselves to be inaccurate. Well, this new box of sensors are showing to be accurate and, so far, long lasting.
Since I've been following an anti-inflammatory diet I've noticed that my infusion sites and sensor sites don't get irritated, and I don't have to remove them at 3 days, or even 6. I have been leaving them in until I begin to notice a loss of function. If my blood sugars run higher than usual it will often prompt an infusion site change and if the sensors become inaccurate I change them as well. However, I've been getting more time than I used to.
I was encouraged to try to see how long a sensor could work by the reports around the diabetes online community that people are getting more time out of their Dexcom or Medtronic sensors. I know it might be a fluke, but, I'm happy to win the min-lottery once in a while. Inserting a CGM sensor is still one of my least favorite activities in my diabetic life. Looking forward to the Enlite, Dexcom G4, and a non-invasive sensor someday.
This week I had a particularly good one. It was comfortable, accurate, and I didn't want to see it go. When the battery ran out I disconnected the battery pack and recharged it. I started it up again and the sensor has continued to be accurate for another week, and I'm still using it on day 12. So, yes, with a battery recharge, the enzymes in the sensor have been able to keep working 4X longer than the stated life.
In my last blog post I was talking about the fact the box of expired sensors I was using were showing themselves to be inaccurate. Well, this new box of sensors are showing to be accurate and, so far, long lasting.
Since I've been following an anti-inflammatory diet I've noticed that my infusion sites and sensor sites don't get irritated, and I don't have to remove them at 3 days, or even 6. I have been leaving them in until I begin to notice a loss of function. If my blood sugars run higher than usual it will often prompt an infusion site change and if the sensors become inaccurate I change them as well. However, I've been getting more time than I used to.
I was encouraged to try to see how long a sensor could work by the reports around the diabetes online community that people are getting more time out of their Dexcom or Medtronic sensors. I know it might be a fluke, but, I'm happy to win the min-lottery once in a while. Inserting a CGM sensor is still one of my least favorite activities in my diabetic life. Looking forward to the Enlite, Dexcom G4, and a non-invasive sensor someday.
Monday, September 24, 2012
Expired sensors: I'm stubborn and frugal, but...
Right after I posted about trusting my sensors enough to use them for corrections... I went on a run of 3-4 sensors that just didn't have it. I wonder if there is something about body chemistry that throws them off. I had such good results for a long time, and the sensors were even expired... More recently I had to toss out the box I was using because they were consistently inconsistent. Yes, they were expired, but that's not always a deal breaker.
The straw that broke the camel's back... I was doing weekend work (catering) which included a lot of hustling and moving of somewhat heavy stuff. My sensor showed me going up, and showed me at 150 mg/dl. Since I've been fighting a cold and running higher BG it' didn't seem that strange to be climbing while being active. I felt more on the low side with a jittery-ness that didn't feel high at all. I tested and found that I was 44 mg/dl. By the time I tested, my sensor was reading 180 mg/dl. So, not only was it off by a lot, it was actually showing movement in the wrong direction. Times like that, you just want to turn it off because it's no help, and you are getting false alarms.
This brings me back to my theory about body chemistry. I have read that Dex sensors are made inaccurate by using acetaminophen. Could there be things in my sinus spray that enter my system and cause my interstitial fluid to less readable by the sensor?
I've also been seeing my sensor stay the same while my meter shows an upward trend for over an hour. So, anyway, I've tossed out the box of sensors that expired in February and now I'm using a box that only expired in June. Why do I have so many expired sensors around? Because I found that I'm able to get 6-7 days on them, doubling their life. Putting them in once a week is a really good trade-off of pain and bruising to useful data. When the data is useless, you wonder...
The straw that broke the camel's back... I was doing weekend work (catering) which included a lot of hustling and moving of somewhat heavy stuff. My sensor showed me going up, and showed me at 150 mg/dl. Since I've been fighting a cold and running higher BG it' didn't seem that strange to be climbing while being active. I felt more on the low side with a jittery-ness that didn't feel high at all. I tested and found that I was 44 mg/dl. By the time I tested, my sensor was reading 180 mg/dl. So, not only was it off by a lot, it was actually showing movement in the wrong direction. Times like that, you just want to turn it off because it's no help, and you are getting false alarms.
This brings me back to my theory about body chemistry. I have read that Dex sensors are made inaccurate by using acetaminophen. Could there be things in my sinus spray that enter my system and cause my interstitial fluid to less readable by the sensor?
I've also been seeing my sensor stay the same while my meter shows an upward trend for over an hour. So, anyway, I've tossed out the box of sensors that expired in February and now I'm using a box that only expired in June. Why do I have so many expired sensors around? Because I found that I'm able to get 6-7 days on them, doubling their life. Putting them in once a week is a really good trade-off of pain and bruising to useful data. When the data is useless, you wonder...
Wednesday, September 5, 2012
Breaking the Rules
I've become a loyal CGMS user. I rarely go for 12 hours without it. I've found that the few times I've cruised around without a sensor, I have some sort of surprise that takes me out of range. I believe that being able to head off a rise when I hit 130 mg/dl makes a big difference. My body is much more nimble and able to get the correction done if I'm still close to the normal range when I correct.
I've found that my CGMS data has been really accurate from 80-160 mg/dl. Like, when I cross-check it with my meter it's wicked close. I don't know if Medtronic updated their sensors, or if my personal chemistry is just jibing with the sensors better, but over the last few months I have been rather impressed, and have grown to trust those numbers on the display.
So, what I've been doing lately is breaking the rules.
You aren't supposed to base corrections on your CGMS reading. It's usually 20 minutes behind your actual BG, and could allegedly be wrong. But, lately, when I see myself hitting a predictable post-meal 130-140 mg/dl I bolus a unit on my pump. It turns it around.
I've written blog posts about the inherent inaccuracy of my CGMS and about how it would never be smart to respond with insulin to the wacky readings you sometimes get. But, I've noticed that things have changed, and I've changed my habits. One thing that makes it work for me is that the dose is small and the correction is timely. If it's post-meal and it's predictable, I'm comfortable with the scenario.
I wouldn't recommend this to anyone else. We all do things off-label that we consider safe, like re-using lancets, and pen needles. And, this is something that I've changed recently. If my BG gets really high (160+) I do the standard meter-check and correct.
But, this has given me a taste of what it might be like when CGMs are really accurate and you or the pump can use the data directly for minute-to-minute corrections, in real time. I'm down with it.
Ironic. I wrote this post a few days ago, and now my current sensor is doing those devious things that I thought were a thing of the past. It's diving and climbing randomly, meanwhile my meter tells me things are as stable and predictable as ever. Hmmm. I guess if you want some good thing to dissolve, you just have to blog about it.
I've found that my CGMS data has been really accurate from 80-160 mg/dl. Like, when I cross-check it with my meter it's wicked close. I don't know if Medtronic updated their sensors, or if my personal chemistry is just jibing with the sensors better, but over the last few months I have been rather impressed, and have grown to trust those numbers on the display.
So, what I've been doing lately is breaking the rules.
You aren't supposed to base corrections on your CGMS reading. It's usually 20 minutes behind your actual BG, and could allegedly be wrong. But, lately, when I see myself hitting a predictable post-meal 130-140 mg/dl I bolus a unit on my pump. It turns it around.
I've written blog posts about the inherent inaccuracy of my CGMS and about how it would never be smart to respond with insulin to the wacky readings you sometimes get. But, I've noticed that things have changed, and I've changed my habits. One thing that makes it work for me is that the dose is small and the correction is timely. If it's post-meal and it's predictable, I'm comfortable with the scenario.
I wouldn't recommend this to anyone else. We all do things off-label that we consider safe, like re-using lancets, and pen needles. And, this is something that I've changed recently. If my BG gets really high (160+) I do the standard meter-check and correct.
But, this has given me a taste of what it might be like when CGMs are really accurate and you or the pump can use the data directly for minute-to-minute corrections, in real time. I'm down with it.
Ironic. I wrote this post a few days ago, and now my current sensor is doing those devious things that I thought were a thing of the past. It's diving and climbing randomly, meanwhile my meter tells me things are as stable and predictable as ever. Hmmm. I guess if you want some good thing to dissolve, you just have to blog about it.
Tuesday, September 4, 2012
August Averages, etcetera
I've downloaded my sensor and pump data and the numbers are kind of average. It seems like I've settled into a cost/benefit ratio for my d-management that works. I'm putting in a tolerable, habitual effort and getting fairly satisfactory results. Things haven't changed much in the last three summer months. I haven't been obsessing too much and haven't tweaked my routine too much.
Sensor average for August: 134 mg/dl
Standard Deviation: 42
Insulin TDD: 25.8 units
Food
As, I looked over my numbers, graphs and charts I can see that I'm still spending more time out of range during the hours after dinner. I'll work on that. I usually consume a decent chunk of protein with dinner and I think I have some kinks to work out with how the protein effects my BG later in the evening. I normally convert protein to an equivalent number of carbs, but it doesn't always work out perfectly. I know I could get into using TAG, but I've never been an absolute engineer about it. Is that okay? Maybe.
Routine & Exercise
Going back to work this month brought some routine back into my life, and it seems that it improved my glucose control too. I stopped my twice daily walks and increased my basal from 14 units to 18 units. It seems to be the right amount for compensating for that activity. I have plantar fasciitis, likely caused by incorrect footwear, so I'm giving my feet some time to recuperate while I'm busy with the Fall schedule. When I see some improvement, I'll make an effort to get some shoes that fit correctly and start my walking again.
Stress
As I returned to work I had planned to respond to increased stress with some basal adjustments. It seems that the basal adjustment that I made for less exercise was also enough to keep things in check for any additional stress from work. Mostly I find that I have some positive adrenaline responses (exhilaration?) from work.
Symlin Update:
First, the spelling: I had previously been spelling it wrong with an extra "i". And, apparently, so had much of the internet, if you search Symilin you will find plenty of discussion... Oops, I just noticed that most of the mispellers are me.)
I did have one episode recently with a-fib. It lasted over 12 hours which was starting to bother me. I worked a weekend evening, catering a wedding, and didn't take my evening dose of beta-blocker till I got home late. I was in a-fib all night and the next AM till about 10am, in church it finally subsided. It was uncomfortable. I felt like my whole torso was being jarred by my jumpy heart. The only trigger that I can point to is the exertion of lots of work and dehydration, and a couple bites of a cookie, which is not on my normal list of foods. I have noticed symptoms after small amounts of gluten containing foods in the past, and I think that cookie might have been enough. I'm willing to do pretty much anything to avoid those drawn out episodes.
Endo time
I think the next time I see my primary physician I will ask for a referral to an endocrinologist. I think my doc has done a great job with me, but I'd love to get a bit closer to the cutting edge studies and see what types of tests they might run to be more proactive with me. I don't want to offend my doctor that's been treating me and calling me his model patient for 12 years, but, you have to do what you have to do...
Sensor average for August: 134 mg/dl
Standard Deviation: 42
Insulin TDD: 25.8 units
Food
As, I looked over my numbers, graphs and charts I can see that I'm still spending more time out of range during the hours after dinner. I'll work on that. I usually consume a decent chunk of protein with dinner and I think I have some kinks to work out with how the protein effects my BG later in the evening. I normally convert protein to an equivalent number of carbs, but it doesn't always work out perfectly. I know I could get into using TAG, but I've never been an absolute engineer about it. Is that okay? Maybe.
Routine & Exercise
Going back to work this month brought some routine back into my life, and it seems that it improved my glucose control too. I stopped my twice daily walks and increased my basal from 14 units to 18 units. It seems to be the right amount for compensating for that activity. I have plantar fasciitis, likely caused by incorrect footwear, so I'm giving my feet some time to recuperate while I'm busy with the Fall schedule. When I see some improvement, I'll make an effort to get some shoes that fit correctly and start my walking again.
Stress
As I returned to work I had planned to respond to increased stress with some basal adjustments. It seems that the basal adjustment that I made for less exercise was also enough to keep things in check for any additional stress from work. Mostly I find that I have some positive adrenaline responses (exhilaration?) from work.
Symlin Update:
First, the spelling: I had previously been spelling it wrong with an extra "i". And, apparently, so had much of the internet, if you search Symilin you will find plenty of discussion... Oops, I just noticed that most of the mispellers are me.)
- I'm almost always taking it after a meal. It seems to work just as well if it's taken 10-15 minutes post-meal.
- I've also found that it helps with corrections at times. If I start a meal with BG above my ideal range, just the introduction of Symlin will cause a drop in glucose. I believe that it is because Symlin impacts the amount of glucose the liver is releasing. With a reduction in liver glucose, there is a drop in BG just from basal insulin and any insulin on board. I have seen discussion on Symlin corrections (see the section titled "how to really screw it up", in which Symlin is taken with a correction bolus and the two hormones work together to provide a rapid correction. I'm rather cautious, and normally don't use any insulin during the hour that Symlin is in my system, but it seems to work to effectively lower glucose all the same.
- Symlin is touted to cause weight loss. I have lost about 10 lbs. since starting Symlin in April. I have dipped below my goal weight and continued to further lean out. I am now making an effort to eat plenty of calories, specifically protein, to support muscle gain. I can't really attribute the weight loss wholly to the Symlin, but, it is one of several factors.
- One bummer is that the last couple times I have purchased Symiln I have paid the same co-pay and gotten 2/3-1/2 the quantity that I'm supposed to get. This was due to insurance schedule limits or pharmacy stock. The co-pay isn't small, so I'm hoping that this will get straightened out. If I'm paying $45 for only 10 days of Symlin, I might start to question how necessary it is.
I did have one episode recently with a-fib. It lasted over 12 hours which was starting to bother me. I worked a weekend evening, catering a wedding, and didn't take my evening dose of beta-blocker till I got home late. I was in a-fib all night and the next AM till about 10am, in church it finally subsided. It was uncomfortable. I felt like my whole torso was being jarred by my jumpy heart. The only trigger that I can point to is the exertion of lots of work and dehydration, and a couple bites of a cookie, which is not on my normal list of foods. I have noticed symptoms after small amounts of gluten containing foods in the past, and I think that cookie might have been enough. I'm willing to do pretty much anything to avoid those drawn out episodes.
Endo time
I think the next time I see my primary physician I will ask for a referral to an endocrinologist. I think my doc has done a great job with me, but I'd love to get a bit closer to the cutting edge studies and see what types of tests they might run to be more proactive with me. I don't want to offend my doctor that's been treating me and calling me his model patient for 12 years, but, you have to do what you have to do...
Tuesday, August 14, 2012
July Health Summary
My July was variable. I had a higher average glucose than I usually do. I'm okay with it. I had a great month with camp, varied activities, varied sleep and food, experiments with donating blood. All worthy pursuits, I guess...
Okay, on with the July numbers.
My average sensor BG was 136 mg/dl.
Standard Deviation was 50.
Average TDD for insulin was 24 units.
Blood Donation Experiment:
I donated blood in early July. I thought that perhaps my BG would be more stable. Studies have shown a connection between iron levels and insulin resistance. I thought that perhaps donating blood would improve my insulin sensitivity and lower my insulin needs. Not this time...
I didn't find that to be true. If anything, I found that it made my glucose levels more variable and unpredictable. I felt that I was more sensitive to carbohydrates. (a caveat: as always, if you have your dosage and correction factors up-ended by a physiological change, it can certainly make your glucose levels less predictable) For me it seemed like it was more than a factor that rocked the boat, it seemed like it actually made my levels less stable all around. I wouldn't discourage anyone from donating blood, but I would say that your results may vary. I plan to do it again, but not to gain any advantages in BG control, just to donate.
Travel & Food Variables:
I went to camp with my kids and ate camp food, left my supplements at home, and battled it out with my glucose meter. I think the absence of my supplements (insulin mimetics) made a difference for a day or two. Once my body got used to the absence I was able to control my BG again. For the first couple days at camp I was averaging about 150 mg/dl. Even with eating less than usual, sometimes skipping meals I was running high-ish. By day three I saw a return to normalcy and felt that I was back on track. I think I can adjust to life without those supplements. I had wondered if my basal and correction factors were dependent on those supplements being in the mix.
At the end of the month I took a quick trip to the Pacific North West. The stress and excitement of travel rattled my nerves enough to show an upward fluctuation in my sugar levels. The whole time I traveled it was a bit off, but there were no significant lows or highs. I guess I'm really a creature of habit and depend on my sleep, daily walks and activity to keep things in check.
Things to keep an eye on:
I have had a few days during the last month in which I felt very tired and fatigued. My motivation was very low and I felt socially and physically spent. Sometimes it lasted up to 2 days, and it seemed more common when I didn't do my AM walk due to schedule.
For two weeks in the middle of the month I have had very itchy skin, all over. The skin is not inflamed and does not show a rash. It just itches like the dickens. At first I thought it was from flea bites or something, but there is no focal point of the itching, no welts, and no redness.
The two things above can be related to thyroid function, so it's still on my radar for possible issues. I've been feeling well otherwise. Although these symptoms have passed, I'm recording it because I want to make sure I keep track of them accurately up till I see my doctor in October. He is taking a conservative stance on thyroid interventions.
Cardiology
I saw my cardiologist toward the end of the month. He didn't have much to tell me, but he's a good listener. He said there was another drug for atrial fibrillation that I might like more than beta-blockers. He said it's like the ideal medication because the side-effects are almost nil and it works well. I don't seem to have any trouble with beta-blockers (well, except maybe the item mentioned in the next paragraph), but it might be interesting to try it and see if my energy is better. My primary doctor has mentioned that the beta blocker might be what is making me feel lethargic periodically.
Additionally, we discussed orthostatic hypotension. In the past several months I have noticed that when I stand up suddenly I get light-headed for about 2 seconds and have to wait for it to pass. I think it is has to do with the beta blocker lowering my blood pressure, which was already on the lower side. He seemed to think it was pretty normal, and didn't think I should worry about. Admittedly I've gotten used to it, and I've never blacked out.
I asked him if he thought I should see an endocrinologist since I have thyroid, diabetic and cardio issues to look after. He said he didn't think it was necessary. My primary care doctor seems to be doing all the things that are needed. At least, I asked. So far, I've gone for 12 years without seeing a legit endo. My primary care doctor (an internist) has been willing to work with me and go in the direction that I'm interested in. It seems to work well for me because he trusts my knowledge and interest in getting good glucose control.
Okay, on with the July numbers.
My average sensor BG was 136 mg/dl.
Standard Deviation was 50.
Average TDD for insulin was 24 units.
Blood Donation Experiment:
I donated blood in early July. I thought that perhaps my BG would be more stable. Studies have shown a connection between iron levels and insulin resistance. I thought that perhaps donating blood would improve my insulin sensitivity and lower my insulin needs. Not this time...
I didn't find that to be true. If anything, I found that it made my glucose levels more variable and unpredictable. I felt that I was more sensitive to carbohydrates. (a caveat: as always, if you have your dosage and correction factors up-ended by a physiological change, it can certainly make your glucose levels less predictable) For me it seemed like it was more than a factor that rocked the boat, it seemed like it actually made my levels less stable all around. I wouldn't discourage anyone from donating blood, but I would say that your results may vary. I plan to do it again, but not to gain any advantages in BG control, just to donate.
Travel & Food Variables:
I went to camp with my kids and ate camp food, left my supplements at home, and battled it out with my glucose meter. I think the absence of my supplements (insulin mimetics) made a difference for a day or two. Once my body got used to the absence I was able to control my BG again. For the first couple days at camp I was averaging about 150 mg/dl. Even with eating less than usual, sometimes skipping meals I was running high-ish. By day three I saw a return to normalcy and felt that I was back on track. I think I can adjust to life without those supplements. I had wondered if my basal and correction factors were dependent on those supplements being in the mix.
At the end of the month I took a quick trip to the Pacific North West. The stress and excitement of travel rattled my nerves enough to show an upward fluctuation in my sugar levels. The whole time I traveled it was a bit off, but there were no significant lows or highs. I guess I'm really a creature of habit and depend on my sleep, daily walks and activity to keep things in check.
Things to keep an eye on:
I have had a few days during the last month in which I felt very tired and fatigued. My motivation was very low and I felt socially and physically spent. Sometimes it lasted up to 2 days, and it seemed more common when I didn't do my AM walk due to schedule.
For two weeks in the middle of the month I have had very itchy skin, all over. The skin is not inflamed and does not show a rash. It just itches like the dickens. At first I thought it was from flea bites or something, but there is no focal point of the itching, no welts, and no redness.
The two things above can be related to thyroid function, so it's still on my radar for possible issues. I've been feeling well otherwise. Although these symptoms have passed, I'm recording it because I want to make sure I keep track of them accurately up till I see my doctor in October. He is taking a conservative stance on thyroid interventions.
Cardiology
I saw my cardiologist toward the end of the month. He didn't have much to tell me, but he's a good listener. He said there was another drug for atrial fibrillation that I might like more than beta-blockers. He said it's like the ideal medication because the side-effects are almost nil and it works well. I don't seem to have any trouble with beta-blockers (well, except maybe the item mentioned in the next paragraph), but it might be interesting to try it and see if my energy is better. My primary doctor has mentioned that the beta blocker might be what is making me feel lethargic periodically.
Additionally, we discussed orthostatic hypotension. In the past several months I have noticed that when I stand up suddenly I get light-headed for about 2 seconds and have to wait for it to pass. I think it is has to do with the beta blocker lowering my blood pressure, which was already on the lower side. He seemed to think it was pretty normal, and didn't think I should worry about. Admittedly I've gotten used to it, and I've never blacked out.
I asked him if he thought I should see an endocrinologist since I have thyroid, diabetic and cardio issues to look after. He said he didn't think it was necessary. My primary care doctor seems to be doing all the things that are needed. At least, I asked. So far, I've gone for 12 years without seeing a legit endo. My primary care doctor (an internist) has been willing to work with me and go in the direction that I'm interested in. It seems to work well for me because he trusts my knowledge and interest in getting good glucose control.
Thursday, July 19, 2012
Post-retro numbers June
For some reason I wasn't focused on summarizing my results when June ended, so it's taken me till now to get this stuff wrapped up. I'll just blame it on the lack of rain. We just had our first real thunderstorm last night and I feel motivated to get caught up.
The reason I write up a health summary every month isn't because I think my readers are really interested in the minutiae. I have found, over time, that I forget how things have changed for the worse or the better. Having monthly check-points helps me to look back and see if I'm moving in the right direction.
Because my memory is impressionistic, I only vaguely remember what June was like in the BG realm. I uploaded my data and saved it for this reason. So, I'm now digging into that data I saved.
Average BG for June was: 123 mg/dl.
Standard deviation for June was: 43.
I'm pretty sure this is one of the higher ones I've recorded. It means I had a decent amount of variability in my blood sugar levels and that I was swinging a bit more than usual. I think July will be even worse because of the impact of blood donation, and less routine in the summer lifestyle.
In the second half of June my average insulin usage per day was 25 units, with 17.5 being basal and 7.5 being bolus. On my most physically active days I have used as little as 19 units.
I did not do an at-home A1C test in June.
I don't think I will continue to do them monthly because the data is redundant with my sensor data. Also, the cost for them at the pharmacy has gone up to $25 per test. As long as there are some questions to the accuracy of the test related to hemoglobin status and red blood cell life, I think sensor data is more valuable. I don't think it will be too many years before other tests and data types eclipse the A1c.
Other factors:
Exercise: In summer I have been able to go for walks twice a day, which has added some stability in the meal and insulin department. It has helped to rapidly correct rises that I've had. It's also produced a few mild lows that had to be corrected. The standard deviation reflects some of that business.
Food: I have been eating breakfast more often during the summer. Taking an AM walk will often get me hungry and cause BG to drop a bit. So, this required me to watch the post-prandial readings for 3 meals most days instead of 2. I love breakfast, so I'm not complaining...
I have experimented with non-wheat carbs after exercise. I have read that after you deplete glycogen, your body can use a ready source of glucose for replenishment. It's the best time to have your glucose. I have used a small amount of potato, sweet potato and the occasional corn tortilla for this and it has usually worked out okay. Sometimes my body still responds too quickly to fast-acting carbohydrates, regardless to the time of day or exercise context.
Sleep: For the month of June I woke up from sun hitting my eyelids, which was generally about 6AM. I generally got enough sleep, but whenever I stayed up past 10PM with the summer family, I was getting less than optimal sleep. I have found that it shows in my BG average the next day or so when I skimp on sleep.
Symilin: I am still using Symilin with every meal. A couple times when we had special meals (Father's Day steaks and Anniversary dinner out) and I took Symilin before the meal I was disappointed when I sat down to eat and could barely stand to eat anything. I've started to take Symilin half way through the meal or just after if I plan on eating a lot. When I've skipped Symilin with breakfast I've noticed a rise that seems disproportionate to the meal. So, I think once your body is used to having Symilin with food, you are acclimated and should be consistent with it.
Weight: I plan on writing a separate post about weight management soon, but I have arrived at my weight goal that I set last summer. I am staying stable at 150 lbs. I am doing some work to gain muscle, but I have gotten to the level of leanness that is appropriate for my frame. It took me almost a year to lose about 18 pounds. I think some of my success in this area has had to do with every factor discussed above, plus daily sun exposure.
The reason I write up a health summary every month isn't because I think my readers are really interested in the minutiae. I have found, over time, that I forget how things have changed for the worse or the better. Having monthly check-points helps me to look back and see if I'm moving in the right direction.
Because my memory is impressionistic, I only vaguely remember what June was like in the BG realm. I uploaded my data and saved it for this reason. So, I'm now digging into that data I saved.
Average BG for June was: 123 mg/dl.
Standard deviation for June was: 43.
I'm pretty sure this is one of the higher ones I've recorded. It means I had a decent amount of variability in my blood sugar levels and that I was swinging a bit more than usual. I think July will be even worse because of the impact of blood donation, and less routine in the summer lifestyle.
In the second half of June my average insulin usage per day was 25 units, with 17.5 being basal and 7.5 being bolus. On my most physically active days I have used as little as 19 units.
I did not do an at-home A1C test in June.
I don't think I will continue to do them monthly because the data is redundant with my sensor data. Also, the cost for them at the pharmacy has gone up to $25 per test. As long as there are some questions to the accuracy of the test related to hemoglobin status and red blood cell life, I think sensor data is more valuable. I don't think it will be too many years before other tests and data types eclipse the A1c.
Other factors:
Exercise: In summer I have been able to go for walks twice a day, which has added some stability in the meal and insulin department. It has helped to rapidly correct rises that I've had. It's also produced a few mild lows that had to be corrected. The standard deviation reflects some of that business.
Food: I have been eating breakfast more often during the summer. Taking an AM walk will often get me hungry and cause BG to drop a bit. So, this required me to watch the post-prandial readings for 3 meals most days instead of 2. I love breakfast, so I'm not complaining...
I have experimented with non-wheat carbs after exercise. I have read that after you deplete glycogen, your body can use a ready source of glucose for replenishment. It's the best time to have your glucose. I have used a small amount of potato, sweet potato and the occasional corn tortilla for this and it has usually worked out okay. Sometimes my body still responds too quickly to fast-acting carbohydrates, regardless to the time of day or exercise context.
Sleep: For the month of June I woke up from sun hitting my eyelids, which was generally about 6AM. I generally got enough sleep, but whenever I stayed up past 10PM with the summer family, I was getting less than optimal sleep. I have found that it shows in my BG average the next day or so when I skimp on sleep.
Symilin: I am still using Symilin with every meal. A couple times when we had special meals (Father's Day steaks and Anniversary dinner out) and I took Symilin before the meal I was disappointed when I sat down to eat and could barely stand to eat anything. I've started to take Symilin half way through the meal or just after if I plan on eating a lot. When I've skipped Symilin with breakfast I've noticed a rise that seems disproportionate to the meal. So, I think once your body is used to having Symilin with food, you are acclimated and should be consistent with it.
Weight: I plan on writing a separate post about weight management soon, but I have arrived at my weight goal that I set last summer. I am staying stable at 150 lbs. I am doing some work to gain muscle, but I have gotten to the level of leanness that is appropriate for my frame. It took me almost a year to lose about 18 pounds. I think some of my success in this area has had to do with every factor discussed above, plus daily sun exposure.
Tuesday, July 17, 2012
Nice! (and I don't mean Walgreen's generic brand)
Transdermal Glucose Sensor- non-invasive CGM
It's pretty awesome that we might have a painless, puncture-free option for getting constant readings. It's like... THE FUTURE.
But, right now there's a lot of future I'm waiting for...
I'll pass on the diabetes alert dog, my CGM has been sufficiently accurate lately.
Well, let's get real... I'm not really waiting for anything. I might even go low tech for a couple weeks and see how going untethered from my pump goes. The unstructured days of sweating and swimming are a great time for that. Despite diabetes, we have to enjoy the moment, right?
It's pretty awesome that we might have a painless, puncture-free option for getting constant readings. It's like... THE FUTURE.
But, right now there's a lot of future I'm waiting for...
- low glucose suspend feature on pump
- a louder, lower beep on my pump that I can actually hear
- enlite sensor
- closed loop system
- smart insulin
I'll pass on the diabetes alert dog, my CGM has been sufficiently accurate lately.
Well, let's get real... I'm not really waiting for anything. I might even go low tech for a couple weeks and see how going untethered from my pump goes. The unstructured days of sweating and swimming are a great time for that. Despite diabetes, we have to enjoy the moment, right?
Monday, July 16, 2012
Trying to figure out "diabetes advocacy" to the public
Some of the blogs that I read seem to be mainly focused on diabetes advocacy (sometimes whining?). It's about telling the world about what it's like to be diabetic. I'm not entirely sure why this matters, the readers are probably mostly people with diabetes.
As a 27 year diabetic, I don't have much interest in the plight of people with other diseases. I'm sympathetic, but, I'm not driven to learn everything I can about them. I guess I'm self-centered, and I have a limited amount of time for research. If someone is shouting it from the rooftop, how hard it is to have a particular disease, I feel kind of perplexed. What, specifically, do they want ME to DO?
As diabetics (or People With Diabetes if you like that term better), we have our problems that we have to overcome and deal with, but what does it matter what other people know or think about our issues? To me, it seems like another way of making our disease someone else's problem. "It's a hard disease, because no one understands..." It's like being a teenager again, "Nobody understands me... " Will we ever be satisfied with what the average person knows about diabetes? I don't think so...
If we tell everyone that we can eat whatever we want if we dose properly, do we get more research funding? If we tell everyone that hypoglycemia really stinks, do we improve our chances of better insurance coverage? If we get indignant when someone mixes up Type 1 and Type 2, do we get access to better medical devices?
I wonder if sometimes we are distracting ourselves from learning more and being proactive because we focus so much on getting the word out about how d-ifficult it is. I hate to say it, but diabetes is unique among many chronic diseases, in that we have the power to make our lives quite a bit better. I've improved my health over the years, and while the disease still dominates much of my life experience (and, in fact, inspires this blog), I don't see myself as a victim. I feel lucky that diabetes has taught me a lot about myself, and human health. I feel lucky that I have a disease in which choices you make can help you live a better, more normal life.
It's been years since a person that I was with questioned what I ate. In fact, more often than not, people are offering me foods that I choose to gently turn down. That's a subtle advocacy for self determination and showing the non-diabetic public that we can take care of ourselves. I'm usually the first to share about my diabetic experience with people I meet. I try to portray a picture of a person that has learned about the body and that I can take steps to make the most of a life with a chronic disease, which is a important part of my life experience.
For me, the connections that are made with other PWDs are more beneficial than anything that we can forge with the non-diabetic public. We understand each other almost automatically. I love the opportunity to share ideas, results and success with people who are living the same condition that I am.
Don't get me wrong, I want the medical community to know what's important to me as a Type 1 diabetic. I want my voice to be heard and understood to the people that matter.
Wednesday, July 11, 2012
Conflicting studies on blood donation and insulin sensitivity
After posting about my experience (so far) with blood donation I did some searching and found two published studies that seem to have opposite conclusions.
One found that blood donors with lower iron stores did not have any different response to glucose tolerance tests. The other found that those with lower iron stores had higher insulin sensitivity and lower insulin secretion. And a health blogger talks about these issues in depth. Hmmm...
It was hard for me to really tell if they used the same glucose tolerance test. I will keep an eye on my blood sugar measurements over the next couple of weeks and probably donate again in August. I am curious about this.
As a side note: I know that a glucose tolerance test would destroy me (and most T1 diabetics?). Non-diabetic people who eat low-carb/ketogenic often fail glucose tolerance tests. When eating a ketogenic diet you develop a type of insulin resistance in the tissues that spares glucose for the tissues that absolutely need it. For instance, parts of the brain can only run on glucose. So in the scarcity of glucose the tissues will down regulate their glucose absorption to make sure that the glucose is reserved for the tissues that need it. Because of this mechanism, I don't handle changes in my glucose intake very well. I run well on fat and protein, and if I throw more carbs or sugar into my diet I get a disproportionate rise in BG. I have to take more insulin than my carb factor indicates to control fast-acting carbs. I know that I could become acclimated to a higher level of glucose in my system, but I prefer to keep things ketogenic because it's the only way I have been able to achieve stable blood sugars.
What would you do to handle 75 grams of liquid carbs?
One found that blood donors with lower iron stores did not have any different response to glucose tolerance tests. The other found that those with lower iron stores had higher insulin sensitivity and lower insulin secretion. And a health blogger talks about these issues in depth. Hmmm...
It was hard for me to really tell if they used the same glucose tolerance test. I will keep an eye on my blood sugar measurements over the next couple of weeks and probably donate again in August. I am curious about this.
As a side note: I know that a glucose tolerance test would destroy me (and most T1 diabetics?). Non-diabetic people who eat low-carb/ketogenic often fail glucose tolerance tests. When eating a ketogenic diet you develop a type of insulin resistance in the tissues that spares glucose for the tissues that absolutely need it. For instance, parts of the brain can only run on glucose. So in the scarcity of glucose the tissues will down regulate their glucose absorption to make sure that the glucose is reserved for the tissues that need it. Because of this mechanism, I don't handle changes in my glucose intake very well. I run well on fat and protein, and if I throw more carbs or sugar into my diet I get a disproportionate rise in BG. I have to take more insulin than my carb factor indicates to control fast-acting carbs. I know that I could become acclimated to a higher level of glucose in my system, but I prefer to keep things ketogenic because it's the only way I have been able to achieve stable blood sugars.
What would you do to handle 75 grams of liquid carbs?
Tuesday, July 10, 2012
Blood Donation
Last week I donated blood. I had never done it before, because I had always assumed (hoped?) that Type 1 diabetics would be excluded. I decided to give it a go because I had read that there can be some potential health benefits. It's summer and feeling tired for a day or so isn't the end of the world. Plus, saving a life is pretty cool.
The experience went smoothly. I was questioned a bit about my a-fib, but the beta blocker that I'm taking wasn't on the list of prohibited drugs. I wasn't excluded.
I thought the process was pretty easy. It's strange to see a bulging bag of your own blood, but I felt fine during the procedure, and afterwards.
I did make a T1 mistake. I arrived with a BG of 150 mg/dl, to make sure that I was in a comfortable spot as they took a pint. During my donation I saw my blood glucose go down by about 40 points, according to my sensor. It made me a bit jumpy, because I thought it was from the donation, but it was probably just from nerves. People usually have some snacks after giving blood to make sure they feel well. I had a glucose tablet right before donation. And afterwards, I accepted a gluten free snack bar that had 21 grams of carb in it. Even with a bolus, my BG shot up higher than expected, and incredibly quickly. After that I was chasing it, trying to keep it stable.
Blood donation has been known to lower insulin resistance in Type 2 diabetics.
I did not experience any clear benefit in my insulin sensitivity. If anything, I have found that I'm more sensitive to the impact of fast acting carbs. In the week that followed donation I went to camp with my kids and consumed foods that were different than my usual fare. I found that my blood sugars were much more volatile than I expected. There were several factors at play, but it seems like things have been a bit more jumpy. Maybe some of that could be insulin sensitivity coupled with faster absorption of glucose. I'm not a fan of the change. It's been much more difficult to keep things stable. Even as I am home, eating normally, I am still experiencing some strange and unpredictable trends. I will probably need to watch my sensor data and see if there's a basis for adjusting basal or carb/correction factors.
Anyone else know any tricks for post-donation management?
The experience went smoothly. I was questioned a bit about my a-fib, but the beta blocker that I'm taking wasn't on the list of prohibited drugs. I wasn't excluded.
I thought the process was pretty easy. It's strange to see a bulging bag of your own blood, but I felt fine during the procedure, and afterwards.
I did make a T1 mistake. I arrived with a BG of 150 mg/dl, to make sure that I was in a comfortable spot as they took a pint. During my donation I saw my blood glucose go down by about 40 points, according to my sensor. It made me a bit jumpy, because I thought it was from the donation, but it was probably just from nerves. People usually have some snacks after giving blood to make sure they feel well. I had a glucose tablet right before donation. And afterwards, I accepted a gluten free snack bar that had 21 grams of carb in it. Even with a bolus, my BG shot up higher than expected, and incredibly quickly. After that I was chasing it, trying to keep it stable.
Blood donation has been known to lower insulin resistance in Type 2 diabetics.
I did not experience any clear benefit in my insulin sensitivity. If anything, I have found that I'm more sensitive to the impact of fast acting carbs. In the week that followed donation I went to camp with my kids and consumed foods that were different than my usual fare. I found that my blood sugars were much more volatile than I expected. There were several factors at play, but it seems like things have been a bit more jumpy. Maybe some of that could be insulin sensitivity coupled with faster absorption of glucose. I'm not a fan of the change. It's been much more difficult to keep things stable. Even as I am home, eating normally, I am still experiencing some strange and unpredictable trends. I will probably need to watch my sensor data and see if there's a basis for adjusting basal or carb/correction factors.
Anyone else know any tricks for post-donation management?
Saturday, June 30, 2012
Atrial Fibrillation Triggers and Blood Donation
A-Fib Triggers
Once in a while I discuss my latest medical condition, atrial fibrillation. Lately, things have been pretty quiet on that front. But, when you have a quiet baseline, you can start to see things stand out as problems. The suspects I have so far are all foods:
Oddly, coffee doesn't make the list. I have two cups of coffee every morning and my sporadic episodes are never anywhere around that event. I did some reading on an A-Fib site today and discovered that coffee and caffeine have been noted as antiarrhythmic, and shown to improve arrhythmia. That's not true for everyone, but it seems to be true for me, as well as many others.
Blood Donation
I've always steered clear of blood donation because I don't particularly like the experience of having blood drawn. Does anyone? I have always felt like my 2-4 blood draws per year was enough of a "donation", although it lacked the altruism. Well, this year during the blood drive at my school I almost gave blood, but I wasn't too crazy about returning to my classroom with the possibility of feeling woozy. So, I put it off again...
I have heard that donating blood can reduce insulin resistance temporarily. I can hardly resist an experiment (yes, still lacking altruism). I don't really expect much, but I have the luxury of messing around with these things in the summer time. On Monday I'm going to donate blood and see what happens, if anything. I'll report my results, as long as I don't get turned away for a medical reason.
Do any of my T1 readers have anything to share about donating blood? Will I get an artificially low A1C? They say males might want to do it once in a while to keep the red blood cells fresh.
Once in a while I discuss my latest medical condition, atrial fibrillation. Lately, things have been pretty quiet on that front. But, when you have a quiet baseline, you can start to see things stand out as problems. The suspects I have so far are all foods:
- Yerba Mate Tea- I was drinking this all day long every day, and when I discontinued it, my frequent episodes of a-fib stopped abruptly. This is the main culprit. It's my fault, I'm moderation-challenged.
- Dark Chocolate- When I had low blood sugar and indulged in some quality cacao I noticed some heart flutters. It makes sense, but it doesn't make me happy.
- Gluten- I don't eat grains much. However, when I wandered outside my Paleo corral I noticed immediate palpitations from sampling some pizza and eating even just a couple pieces of penne pasta. Crazy small amounts, and very noticeable.
- Black Tea- I'm still willing to experiment with this one. Once, when I tested out a new type of Indian tea that we picked up, I found my heart beating double time almost as soon as I had finished the mug. While it's a stimulant, that response was out of the norm.
- Alcohol- I consume moderate amounts of alcohol almost everyday, but haven't noticed problems consistently. I think my experiences with alcohol may be more related to gluten because beer was often the specific trigger.
Oddly, coffee doesn't make the list. I have two cups of coffee every morning and my sporadic episodes are never anywhere around that event. I did some reading on an A-Fib site today and discovered that coffee and caffeine have been noted as antiarrhythmic, and shown to improve arrhythmia. That's not true for everyone, but it seems to be true for me, as well as many others.
Blood Donation
I've always steered clear of blood donation because I don't particularly like the experience of having blood drawn. Does anyone? I have always felt like my 2-4 blood draws per year was enough of a "donation", although it lacked the altruism. Well, this year during the blood drive at my school I almost gave blood, but I wasn't too crazy about returning to my classroom with the possibility of feeling woozy. So, I put it off again...
I have heard that donating blood can reduce insulin resistance temporarily. I can hardly resist an experiment (yes, still lacking altruism). I don't really expect much, but I have the luxury of messing around with these things in the summer time. On Monday I'm going to donate blood and see what happens, if anything. I'll report my results, as long as I don't get turned away for a medical reason.
Do any of my T1 readers have anything to share about donating blood? Will I get an artificially low A1C? They say males might want to do it once in a while to keep the red blood cells fresh.
Friday, June 29, 2012
Cute posts?
If you saw a couple of adorable digital drawings (hearts and whatnot) posted on this blog with no explanation... well, that was our Penny. She found the Blogger app on the iPad and went ahead and created some content. She thought it was "just a drawing thing". Aw.
She told me to delete them because she had no idea how public this thing was. I didn't even know you could draw directly into blogger. I'm going to have to snoop around, that might be useful some day.
She told me to delete them because she had no idea how public this thing was. I didn't even know you could draw directly into blogger. I'm going to have to snoop around, that might be useful some day.
Wednesday, June 27, 2012
Negative for autoantibodies AND glasses this year...
.JPG) |
| They eventually learned how annoying dialated eyes can be. |
Today we received the results from the Diabetes Trialnet and they were negative for all three kids. It helps that 1/2 of their genes are from my wife who has very few genetic health risks, and no autoimmune diseases that we are aware of. I'm like the clearinghouse of genetic health stuff in my family. We will repeat the test yearly.
We are glad. We can always use the extra time being open an positive about how I manage my glucose. When I interviewed them about diabetes in the winter they forgot that insulin treats high blood sugar and said that if your BG is high you might have to "rest it out". I guess that's how chill I am, I just rest it out (wink). Since then I've been more explicit about how I control my sugar levels. Exercising has been an obvious part of that lately.
As an added bonus, we had their eyes dialated and checked, at the optometrist. The younger two don't need any corrective lenses, yet. I've had a need for glasses since a young age. In fact, I managed to get bi-focals in 3rd grade. As a photography teacher, I can tell you, there are quite a few teens walking around with blurry vision.
Anyway, I'm having a great summer with these three and love the extra time I am able to spend with them during breaks from school. They are really fun, smart, and entertaining. Ellie is taking a trip to the Philippines to visit my parents in about 2 weeks, then starting high school in August. Simon is going to camp for 12 days with his cousins. We are trying to have as much fun together as we can before we end up all over the place.
Tuesday, June 26, 2012
Using exercise against itself
Today I got away with a few things that I normally wouldn't. It was like a triple cheat, triple win. And, I plan to keep doing it whenever I can get away with it.
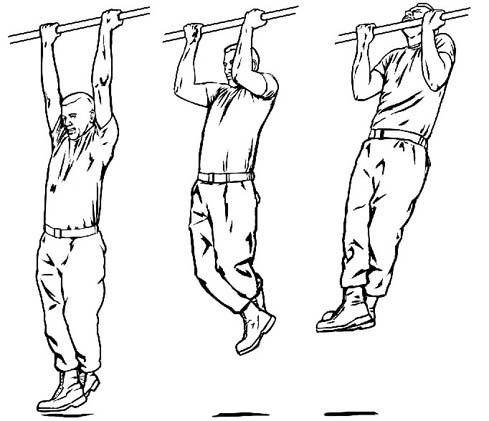
Today, I woke up with normal BG at 94 mg/dl. I had my coffee without a bolus, and then went for a walk. When I got back from my 20 min. walk, my BG was headed toward lowish (70 mg/dl). I did a strength training routine (pushup, pullup, plank, overhead press) which redirected my trend towards normal/steady (104 mg/dl). Both of those activities left me feeling pretty hungry, so I made breakfast. I pondered whether the extra insulin sensitivity from the exercise might allow me to get away with some starch at breakfast. I microwaved a large new potato and then crushed it in the skillet, and drizzled it with coconut oil, and fried it till crispy. I added that to my eggs and greens. It was fantastic, I love potatoes, but rarely eat them because of the fast BG rise that I normally get from them. I used Symilin with the meal, and when I saw my BG starting to go up (at about an hour) I took insulin to cover the meal. It worked out rather well.
I got the idea to combine the walk with the strength training because I had heard that circuit training was sometimes a glucose stabilizing way to exercise because it combined aerobic with anaerobic work and resulted in a balance of BG lowering and raising activities.
I only do strength work about twice a week, so this won't be a daily routine, but it's good to know it works. I wouldn't want to get sick of exercising or occasional potatoes...
- Normally, when I go for a walk in the AM I can skip my 1/2 unit coffee bolus. But, even then, I might dip a little low upon returning from my walk, so I have to eat a glucose tablet or have breakfast with some berries, depending on how low I go.
- If I do a strength workout in the evening I normally see my glucose rise and have had to start taking a unit of insulin to keep it steady.
- My usual breakfast is low-carb, normally eggs and greens. The morning is the time when I have the least leeway with starchy carbs. During the school year I don't really even eat anything till after the dawn phenomenon is over, and it's usually around 11am when I "break the fast".
Today, I woke up with normal BG at 94 mg/dl. I had my coffee without a bolus, and then went for a walk. When I got back from my 20 min. walk, my BG was headed toward lowish (70 mg/dl). I did a strength training routine (pushup, pullup, plank, overhead press) which redirected my trend towards normal/steady (104 mg/dl). Both of those activities left me feeling pretty hungry, so I made breakfast. I pondered whether the extra insulin sensitivity from the exercise might allow me to get away with some starch at breakfast. I microwaved a large new potato and then crushed it in the skillet, and drizzled it with coconut oil, and fried it till crispy. I added that to my eggs and greens. It was fantastic, I love potatoes, but rarely eat them because of the fast BG rise that I normally get from them. I used Symilin with the meal, and when I saw my BG starting to go up (at about an hour) I took insulin to cover the meal. It worked out rather well.
I got the idea to combine the walk with the strength training because I had heard that circuit training was sometimes a glucose stabilizing way to exercise because it combined aerobic with anaerobic work and resulted in a balance of BG lowering and raising activities.
I only do strength work about twice a week, so this won't be a daily routine, but it's good to know it works. I wouldn't want to get sick of exercising or occasional potatoes...
Tuesday, June 19, 2012
T1D Exchange Finds People with Type 1 Diabetes Don’t Meet Targets
I just read Jessica Apple's analysis of the problem with T1 diabetics not being successful in achieving the health that doctors and the ADA desire for them. It hit a chord for me, because I was one of those people "doing everything right" but not getting the prescribed results.
Basically, the study found that a large proportion of Type 1 diabetics are gaining weight and not meeting recommended A1C levels. The question is, will the ADA change their recommendations on diet and insulin? Personally, with kids, I think a higher A1C might be more appropriate, but with adults it seems that if healthy A1C goals can't be achieved, we have to look to the diet in a more aggressive way. If you are keeping your A1Cs in line, not gaining weight, and maintaining your health, then you are doing well.
I added my 2 cents in the comments, but, since it sums up some of my experiences, frustrations and core beliefs about diabetes. I'm going to repeat it here.
Basically, the study found that a large proportion of Type 1 diabetics are gaining weight and not meeting recommended A1C levels. The question is, will the ADA change their recommendations on diet and insulin? Personally, with kids, I think a higher A1C might be more appropriate, but with adults it seems that if healthy A1C goals can't be achieved, we have to look to the diet in a more aggressive way. If you are keeping your A1Cs in line, not gaining weight, and maintaining your health, then you are doing well.
I added my 2 cents in the comments, but, since it sums up some of my experiences, frustrations and core beliefs about diabetes. I'm going to repeat it here.
Here’s the thing… if you have a kidney problem or a gall bladder removed you have a list of foods that you have to avoid to stay healthy. No one really argues with that too much. But, for some reason we have been reticent to tell PWDs (people with serious metabolic issues) that anything is off limits. Let’s get real. Let’s not treat PWDs like little children who might throw a tantrum and give them the info that they really need to be successful. I think, with more success, the issue of depression linked with diabetes could be moderated. Poor control, weight gain, the threat of complications and a constant sense of failure… that’s depressing.
I tried to meet the recommended healthy A1C requirements for years while cooking from scratch, eating all whole foods, but never sorting out the fast acting carbs part of the equation. I never got there. I gained weight, became insulin resistant, and had poor control. Once I started limiting which foods I ate, I was able to make progress in my health goals. It was wicked simple.
The fact is, anyone who uses/creates too much insulin, PWD or not, will have negative impacts in their health. Hyperinsulinemia is a real problem. The ADA needs to encourage people to use less insulin, and therefore eat less foods that require lots of insulin. Good control is within everyone’s reach, but it’s like we/they are afraid to tell the D-community that they can’t have anything they want, all the time. The mantra that we can eat just like everyone else is silly, especially when you see that the rest of the western world (everyone else) is having it’s own insulin related metabolic problems.
Saturday, June 16, 2012
I'll take a flashy new pump with a Dexcom on the side.
After hearing that the tSlim pump would soon be available in the US market, I decided to go to their site and see what they had going on. I knew that they had updated their technology to a level that compares with other devices that we use, like iPhones, and the like. After looking over everything they had, I was pretty interested in their pump. The main things that I liked were the full-color screen, the type of info that is displayed on the home screen, and being rechargeable. But, the thing that most caught my attention was that they are working with Dexcom for sensor integration. I hope that they mean that the pump will act as a Dexcom receiver. That would be excellent.
I requested info from Tandem about their pump and also asked how soon the CGMS integration might be available. I received a reply (from a human being, no less...) and they told me that the work was, indeed, underway, and that it would be available as soon as possible. I know in FDA years that's probably still a while.
If Medtronic doesn't update too much during that time, I'll probably be jumping over to a more colorful display, well thought out design, and sensors that last longer and hurt less.
Meanwhile Medtronic is also working on patch pumps, and they already have a new sensor (also longer lasting, and less painful) going through FDA approval. If you like patch pumps, Omnipod is pretty well received and they are also rumored to be working on CGMS integration with Dexcom. I might like patch pumps, but my favorite infusion sites are places (buttocks!) where I can't discreetly wear a pod.
Anyway, I think it will be a pretty interesting year for some developments in the technology and I hope that the transition to new stuff goes smoothly for insurance, etc. You can only hope.
Thursday, June 7, 2012
Broccoli breakfast
Eating from the garden is probably one of my favorite things in the world. Some coconut oil and red pepper flakes just made the broccoli shine a bit more. When I eat breakfast, this is how I like to do it.

Wednesday, June 6, 2012
Sheepishly I'm a huge fan... of walking.
I can be pretty stubborn.
Something that I've been stubbornly wrong about it that walking is legitimate "exercise". I've always thought it wasn't strenuous enough or cardio enough to make a real fitness difference. Even with all the recommendations from "authorities" to walk more, I had my own theories about it. I thought that encouraging walking was just a "baby-step" to help unfit people get closer to being active. Maybe the thinking was if you could get people to walk more, they might really exercise someday.
Well, through a circuitous route I've landed myself in the "walking is better than" running, or cycling, or jogging, or _____________ camp. When I take a brisk walk, I find that my insulin kicks in and works better, faster. If it can be seen on a CGMS I'm guessing the same things are happening in everyone that walks. For me, seeing the numbers at work has been very eye-opening.
What does walking have that other forms of activity might not?
It's low-impact. You aren't likely to develop injuries from repetitive actions that your body isn't ready for. Since you walk your whole life, it's the most natural way for you to get moving. (One summer I injured my achilles tendon from doing lots of dog-walking in flip-flops, but that was unusually foolhardy.)
It's accessible. You can walk in any clothing you have on (caution with flip-flops recommended). You can walk wherever you are. You can walk with people who don't normally "exercise". The barriers to getting it done are very few.
It's easy, and the heart rate is spot on. How many times have you done a serious run or bike ride and found yourself exercising at a level that makes you feel lousy and sore, and not look forward to doing it again? For me, if I exercise at a heart rate of over 155 bpm, I'm officially working too hard. I find it very hard to dial myself back to that level when I run or cycle. When I walk at a fast pace I don't think it's possible to breech the threshold into unhealthy exercise. We never return from a walk and think "Wow, I'm super exhausted!" From talking to others, I have found that most people tend to exercise above their target heart rate zone, and often are reluctant to get out there for another workout, because, frankly, it was uncomfortable. For this reason many athletes use heart rate monitors to keep themselves in check and keep from working at a rate that is too high. For me walking is always in the low end of the target heart rate window, and I don't need a heart rate monitor to tell me how fast to walk.
It reduces stress instead of causing it.
Excessive or overly strenuous exercise can cause you negative stress that can oftentimes be worse for your body that better. Cortisol (stress hormone) release from strenuous exercise is conter-productive to most people's fitness goals. Walking has very little risk of working against you this way.
Conditioning.
Contrary to what I had previously thought, walking regularly this season has improved my readiness for other activities. Last summer when I began stand up paddling I found that I could only go out for 15-20 minutes before my legs got too shaky to keep going. This year, on my first day out I was able to go out three different times for about an hour without feeling fatigue in my legs. I think it has a lot to do with the regular activity throughout the winter that prepared my legs for long periods of balance work. That was unexpected.
I'm not saying that everyone should stop doing the exercise that they find stimulating and fun, but that for baseline activity walking is safe, easy, accessible and useful. I began exercising much more frequently since I moved walking onto my exercise menu. If I could cycle, rock climb, cross-country ski, stand up paddle, hike, and kayak everyday I would be ecstatic. Until I retire and live in such a paradise, going for one or two 20 minute walks a day has been incredibly helpful in increasing my insulin sensitivity and correcting BG that is headed out of range.
Something that I've been stubbornly wrong about it that walking is legitimate "exercise". I've always thought it wasn't strenuous enough or cardio enough to make a real fitness difference. Even with all the recommendations from "authorities" to walk more, I had my own theories about it. I thought that encouraging walking was just a "baby-step" to help unfit people get closer to being active. Maybe the thinking was if you could get people to walk more, they might really exercise someday.
Well, through a circuitous route I've landed myself in the "walking is better than" running, or cycling, or jogging, or _____________ camp. When I take a brisk walk, I find that my insulin kicks in and works better, faster. If it can be seen on a CGMS I'm guessing the same things are happening in everyone that walks. For me, seeing the numbers at work has been very eye-opening.
What does walking have that other forms of activity might not?
It's low-impact. You aren't likely to develop injuries from repetitive actions that your body isn't ready for. Since you walk your whole life, it's the most natural way for you to get moving. (One summer I injured my achilles tendon from doing lots of dog-walking in flip-flops, but that was unusually foolhardy.)
It's accessible. You can walk in any clothing you have on (caution with flip-flops recommended). You can walk wherever you are. You can walk with people who don't normally "exercise". The barriers to getting it done are very few.
It's easy, and the heart rate is spot on. How many times have you done a serious run or bike ride and found yourself exercising at a level that makes you feel lousy and sore, and not look forward to doing it again? For me, if I exercise at a heart rate of over 155 bpm, I'm officially working too hard. I find it very hard to dial myself back to that level when I run or cycle. When I walk at a fast pace I don't think it's possible to breech the threshold into unhealthy exercise. We never return from a walk and think "Wow, I'm super exhausted!" From talking to others, I have found that most people tend to exercise above their target heart rate zone, and often are reluctant to get out there for another workout, because, frankly, it was uncomfortable. For this reason many athletes use heart rate monitors to keep themselves in check and keep from working at a rate that is too high. For me walking is always in the low end of the target heart rate window, and I don't need a heart rate monitor to tell me how fast to walk.
It reduces stress instead of causing it.
Excessive or overly strenuous exercise can cause you negative stress that can oftentimes be worse for your body that better. Cortisol (stress hormone) release from strenuous exercise is conter-productive to most people's fitness goals. Walking has very little risk of working against you this way.
Conditioning.
Contrary to what I had previously thought, walking regularly this season has improved my readiness for other activities. Last summer when I began stand up paddling I found that I could only go out for 15-20 minutes before my legs got too shaky to keep going. This year, on my first day out I was able to go out three different times for about an hour without feeling fatigue in my legs. I think it has a lot to do with the regular activity throughout the winter that prepared my legs for long periods of balance work. That was unexpected.
I'm not saying that everyone should stop doing the exercise that they find stimulating and fun, but that for baseline activity walking is safe, easy, accessible and useful. I began exercising much more frequently since I moved walking onto my exercise menu. If I could cycle, rock climb, cross-country ski, stand up paddle, hike, and kayak everyday I would be ecstatic. Until I retire and live in such a paradise, going for one or two 20 minute walks a day has been incredibly helpful in increasing my insulin sensitivity and correcting BG that is headed out of range.
Sunday, June 3, 2012
High intensity muscle work, a new tricky project...
I've been doing some sporadic strength training, but the frequency has been spotty because the effect on BG has been hard to predict and balance. The first time I did a 30 min. workout before dinner (a couple months ago) I ended up with my BG at 300 after dinner. Geesh, talk about counter-intuitive results...
Yesterday, I took a unit of insulin before working out and then had dinner, and saw it rise to 170 mg/dl before I took a walk and another correction and it began to descend.
I also threw in another variable which was that I had a glass of milk with dinner, which is usually "off my list". I understand that the carbs and other parts of the milk might be useful post-workout to help with recovery and muscle building. It's likely that I didn't bolus enough for the milk and the meal together. I was shy on the bolus because of the insulin sensitivity that often comes after exercise. I normally think of a glass of milk as 12 grams of carb, which is about what I usually eat for my whole meal. I only bolused for 15 grams.
In the end, I spent the 7pm-midnight window out of range, and a correction at about 9:30pm brought things back to normal overnight. I looks like I needed about 1.5 more units somewhere in the mix. The caveat... I'm not sure I would want to bolus much more in this situation because my wake-up BG was 50-60 mg/dl. I think the exercise impacted my overnight basal. There are surely a few moving parts here.
I may try working out earlier in the day so that I can isolate the impact and get it straightened out before it gets tangled in meal and bedtime factors. It's a bit tricky because the AM isn't probably the best time to do strength training because of the dawn phenomenon, but the pre-dinner window is also less than perfect. Well, just until I get it sorted out... and I will.
Yesterday, I took a unit of insulin before working out and then had dinner, and saw it rise to 170 mg/dl before I took a walk and another correction and it began to descend.
I also threw in another variable which was that I had a glass of milk with dinner, which is usually "off my list". I understand that the carbs and other parts of the milk might be useful post-workout to help with recovery and muscle building. It's likely that I didn't bolus enough for the milk and the meal together. I was shy on the bolus because of the insulin sensitivity that often comes after exercise. I normally think of a glass of milk as 12 grams of carb, which is about what I usually eat for my whole meal. I only bolused for 15 grams.
In the end, I spent the 7pm-midnight window out of range, and a correction at about 9:30pm brought things back to normal overnight. I looks like I needed about 1.5 more units somewhere in the mix. The caveat... I'm not sure I would want to bolus much more in this situation because my wake-up BG was 50-60 mg/dl. I think the exercise impacted my overnight basal. There are surely a few moving parts here.
I may try working out earlier in the day so that I can isolate the impact and get it straightened out before it gets tangled in meal and bedtime factors. It's a bit tricky because the AM isn't probably the best time to do strength training because of the dawn phenomenon, but the pre-dinner window is also less than perfect. Well, just until I get it sorted out... and I will.
Saturday, June 2, 2012
Getting Outside!

School's not quite out yet, but we've been pretending. We got out for a weeknight bike ride on Tuesday. I like getting in some activity and having it not be so clinical. I haven't been on the elliptical machine in weeks, and the fresh air is really welcome. Hopefully, I'll be able to keep the kids interested all summer, skinned knees and all! Luckily, Penny is the toughest and the most resilient.
Friday, June 1, 2012
May Numbers and Whatnot
 |
| Our strawberry patch really kicked out some fruit this year. |
I think according to my sensor data this past month was one of my best for glucose control. I think getting confident with using Symilin and using regular exercise to become more insulin sensitive has helped a lot.
Numbers
My 30 Day Average BG is 120 with a standard deviation of 39. This means I'm staying mostly between 100 and 140 mg/dl. I would say this is accurate, based on my (somewhat obsessive) CGMS watching.
The at-home-A1C showed 6.3 which comes out to an average glucose value of 134 mg/dl.
I expected a lower A1C value, but I'm coming to the conclusion that I might be at that point where running the numbers any lower would have me in hypo territory much more often. As it is, I'm using a glucose tablets about every other day to keep myself in range.
Insulin
I have adjusted my basal so that my total daily dose is at it's lowest at 23-26 units a day, and sometimes it still seems to be a bit too high. I have lost a few pounds since starting Symilin, so I think insulin sensitivity and less body weight play into that equation.
Exercise
I've found that taking 1-2 brisk walks a day has given me the best return on investment with exercise. I usually take one in the beginning of my work day and then another after dinner. When this has been regular, I see the most consistent BG levels and lowest need for insulin.
Also, in the past, the arrival of warm weather has also tended to lower my insulin demands, so that's probably going on too.
The End of the Yerba Mate Experiment
I was excited about the possibilities that Yerba Mate might offer for metabolism, etc. After drinking it throughout the day for about 6-8 weeks, I decided to stop using it. Why? Well, it started with vanity. It was staining my teeth. But, one of the things that improved when I stopped using it was that my episodes with rapid heart rate reduced in frequency, by a lot. I guess it doesn't take a genius to hypothesize that consuming a stimulant might impact heart rate/rhythm, but I've never claimed to be a genius. So, I went to the dentist and had my teeth buffed back to their normal hue and I'm rarely noticing my pulse being out of whack. It's a win-win. My morning coffee and moderate exercise don't seem to have any impact on my heart rhythms.
Thyroid Questions
Last month I was a bit peeved that my doctor wasn't more aggressive about finding out why my TSH levels were high. I began taking a supplement (Thyroid Energy) and during that time I was also having more noticeable rapid heart rate. I decided to take way less, way less often. So, now if I have a day where I'm feeling really sluggish, despondent, or low energy, I take the supplement the next AM. It seems to help. I've only taken a low dose of it about 3 times in the last month. My energy has been good and I've been feeling good overall. I think it's right that we didn't mess with anything major, and I feel it's wise to use the supplement at the lowest possible dose.
I'm finding it really useful to have these monthly notes so that I can go back and review where I have been. I have already looked back at the previous 4 months a few times when I want to verify my progress. I recommend keeping health summary notes for yourself if you haven't done it.
Labels:
A1C,
amylin,
average glucose,
basal,
exercise,
insulin,
low-carb,
results,
Symilin,
thyroid,
Type 1 diabetes,
yerba mate
Monday, May 28, 2012
My Symilin/ Insulin Routine
So, I've been using Symilin alongside my low-carb way of eating for over a month now and I think I have seen some significant improvements in my glucose control. It's taken a bit of experimentation to figure out what works best, but I had some good info to work from as a starting point.
Timing
I take my Symilin dose between 0-10 minutes before sitting down to eat. Once or twice I took it 20 minutes before eating and after a few bites the "satiety effect" kicked in and I didn't feel like eating as much as I had planned (another reason to bolus after the meal).When I take it close to a meal, I have about 15-20 minutes of serious scarfing before I feel full. Sometimes I don't even notice the satiety effect, but I just eat what I normally do and I'm done.
Food Consistency
It is helpful to eat roughly the same amount of protein and carbohydrate in my meals. I'm not even sure exactly how it measures, but I know what it looks like. For most meals I eat 4-6 oz. of protein and some green veggies or salad. If I eat a meal that is slightly different than this, I just use the same amount and plan to correct if needed. When I'm off, the surplus is usually corrected by an evening walk or a small correction 4 hours post meal. A few times I have used a larger bolus for a meal that seemed larger I have ended up getting lows post-meal. When I have had a more active day or am running lowish all day, I will bolus even less.
Insulin Dose Consistency/ Timing
For this average amount of food, I take 1.8 units of Novolog and spread it out over 60-90 minutes with a square bolus. I change the timing post-meal depending on what my starting BG was. If I start a meal over 100 mg/dl I will take it a bit sooner, sometimes even right after a meal. But, if I start a meal at 70-80 mg/dl I give the food plenty of time to start to bring my glucose up and then take the bolus. This would normally be about an hour post-meal.
Taking Symilin After a Meal
A handful of times I have eaten a meal without taking Symilin (because it wasn't with me at the moment) and I have taken it post meal. I didn't notice any difference. I think the low-carb meals are already slow to impact glucose, so there seems to be some wiggle room there.
Symilin Lows
I have read about people having lows that are hard to correct when using Symilin. The reason they are uniquely tricky is that when your digestion is slowed down, it can be hard to get glucose to be quickly absorbed when correcting a low. This knowledge made me very cautious about my insulin dosages while using Symilin. During the first 2-3 weeks using it I was running my BGs higher than usual out of caution. Over time, I have found that my modest doses of insulin do not cause extreme drops, with or without Symilin. The lows I have had in the 50-60 mg/dl range have been easily corrected with 1-2 glucose tablets. The sugar was absorbed normally, and I saw improvement quickly. I think that a low-carb way of eating helps to avoid some of the risks of difficult hypos because the boluses are kept small.
The results have been good for me. I have had rather flat post-meal numbers and I have been able to reduce my total daily insulin. I'm using about 10-20% less insulin.
Timing
I take my Symilin dose between 0-10 minutes before sitting down to eat. Once or twice I took it 20 minutes before eating and after a few bites the "satiety effect" kicked in and I didn't feel like eating as much as I had planned (another reason to bolus after the meal).When I take it close to a meal, I have about 15-20 minutes of serious scarfing before I feel full. Sometimes I don't even notice the satiety effect, but I just eat what I normally do and I'm done.
Food Consistency
It is helpful to eat roughly the same amount of protein and carbohydrate in my meals. I'm not even sure exactly how it measures, but I know what it looks like. For most meals I eat 4-6 oz. of protein and some green veggies or salad. If I eat a meal that is slightly different than this, I just use the same amount and plan to correct if needed. When I'm off, the surplus is usually corrected by an evening walk or a small correction 4 hours post meal. A few times I have used a larger bolus for a meal that seemed larger I have ended up getting lows post-meal. When I have had a more active day or am running lowish all day, I will bolus even less.
Insulin Dose Consistency/ Timing
For this average amount of food, I take 1.8 units of Novolog and spread it out over 60-90 minutes with a square bolus. I change the timing post-meal depending on what my starting BG was. If I start a meal over 100 mg/dl I will take it a bit sooner, sometimes even right after a meal. But, if I start a meal at 70-80 mg/dl I give the food plenty of time to start to bring my glucose up and then take the bolus. This would normally be about an hour post-meal.
Taking Symilin After a Meal
A handful of times I have eaten a meal without taking Symilin (because it wasn't with me at the moment) and I have taken it post meal. I didn't notice any difference. I think the low-carb meals are already slow to impact glucose, so there seems to be some wiggle room there.
Symilin Lows
I have read about people having lows that are hard to correct when using Symilin. The reason they are uniquely tricky is that when your digestion is slowed down, it can be hard to get glucose to be quickly absorbed when correcting a low. This knowledge made me very cautious about my insulin dosages while using Symilin. During the first 2-3 weeks using it I was running my BGs higher than usual out of caution. Over time, I have found that my modest doses of insulin do not cause extreme drops, with or without Symilin. The lows I have had in the 50-60 mg/dl range have been easily corrected with 1-2 glucose tablets. The sugar was absorbed normally, and I saw improvement quickly. I think that a low-carb way of eating helps to avoid some of the risks of difficult hypos because the boluses are kept small.
The results have been good for me. I have had rather flat post-meal numbers and I have been able to reduce my total daily insulin. I'm using about 10-20% less insulin.
Saturday, May 26, 2012
FastClixing (a longish post about something I didn't know I cared about)
During college in the 90s, I volunteered to be in a diabetes product study group, and the topic of discussion was lancets. We showed up at a hotel conference room in Orange County for a discussion. I was sitting around a table with a bunch of other T1 diabetics (pretty neat) and we were giving our feedback about bloodletting. I distinctly remember two people in the study. One guy was a bit whiney and kept on saying that he didn't like the blood extraction process, because it hurt. He hated being poked. Another older gentleman, more of a cowboy, said he didn't care about anything, except, that it was easy to get blood out of his finger. I was just happy that we were being asked, but I didn't think what we wanted made much difference. These devices pierce your skin and make you bleed, and that's just what they do. I was more on the side of the cowboy, and didn't want to have to milk my finger too much to get a drop of blood out of it.
It wasn't too much longer that we saw varied depth, alternative site, lancing devices, and even thinner lancets come onto the market. I guess they heard our whines.
So, in recent years I've never really thought about my lancing device... I just used it. Whichever one I had... I used whichever one came with the meter, or migrated from another meter case. Like many people with diabetes, I change my lancets maybe once a month, when it seems to hurt more than usual. I have never had an infection on a test site on a finger. Have you?
Enter FastClix... my new meter came with a FastClix lancing device (lancer?). I mentioned in a previous post that loading the lancets and starting to use it was different. I think it is well designed and functions well, so I will highlight a few things I like about it.
Six lancet drum
It seems like a rotating drum of 6 lancets like that would be massive and bulky, but they've squeezed 6 pieces of thin, skin piercing tips into a small package. It is only barely larger than your normal lancet, and contains 6 fresh stiletto type lancets that pop up when needed. Even better, they load in and out of your device without exposed points ever being seen or touched. Clever.
Lancet changes
To change tips you slide a lever across, and, voila, you have a new lancet installed. So, if you continue to change them once a month, you might find yourself only thinking about replenishing lancets a couple times a year. Then again, since it's not a pain anymore, you might do it more often. I've already switched to my second one, and I've only been using the thing for a week.
Lancing Depth Options
It has 11 depth options (shown as .5-5.5). The instructions suggest that you start with 2 if you have "soft skin". Since I don't really use the pads of my fingers as much, I qualify as a soft skinned fellow. I was using the 1.5 setting and getting plenty of juice.
Fast
Something about the way it touches your finger is gentler and faster than other lancing devices. It doesn't have the same type of blunt force that my previous lancing devices have had. It's hard to describe, but I've always felt the device throwing it's weight around inside the chassis and my finger was always receiving that tiny slam.
Pain
This is the sneaky part. I thought any method for making a hole in your finger that would bleed sufficiently would pretty much trigger the same pain receptors. Not true. I was shocked the first couple of times I used it, I barely felt the thing graze my skin and it made a nice bleeding hole. It was like witchcraft. Every time I used it I would mentally say, "Cool!"
Design
There are two design points that I want to compliment the FastClix engineers on.
It wasn't too much longer that we saw varied depth, alternative site, lancing devices, and even thinner lancets come onto the market. I guess they heard our whines.
So, in recent years I've never really thought about my lancing device... I just used it. Whichever one I had... I used whichever one came with the meter, or migrated from another meter case. Like many people with diabetes, I change my lancets maybe once a month, when it seems to hurt more than usual. I have never had an infection on a test site on a finger. Have you?
Enter FastClix... my new meter came with a FastClix lancing device (lancer?). I mentioned in a previous post that loading the lancets and starting to use it was different. I think it is well designed and functions well, so I will highlight a few things I like about it.
Six lancet drum
It seems like a rotating drum of 6 lancets like that would be massive and bulky, but they've squeezed 6 pieces of thin, skin piercing tips into a small package. It is only barely larger than your normal lancet, and contains 6 fresh stiletto type lancets that pop up when needed. Even better, they load in and out of your device without exposed points ever being seen or touched. Clever.
Lancet changes
To change tips you slide a lever across, and, voila, you have a new lancet installed. So, if you continue to change them once a month, you might find yourself only thinking about replenishing lancets a couple times a year. Then again, since it's not a pain anymore, you might do it more often. I've already switched to my second one, and I've only been using the thing for a week.
Lancing Depth Options
It has 11 depth options (shown as .5-5.5). The instructions suggest that you start with 2 if you have "soft skin". Since I don't really use the pads of my fingers as much, I qualify as a soft skinned fellow. I was using the 1.5 setting and getting plenty of juice.
Fast
Something about the way it touches your finger is gentler and faster than other lancing devices. It doesn't have the same type of blunt force that my previous lancing devices have had. It's hard to describe, but I've always felt the device throwing it's weight around inside the chassis and my finger was always receiving that tiny slam.
Pain
This is the sneaky part. I thought any method for making a hole in your finger that would bleed sufficiently would pretty much trigger the same pain receptors. Not true. I was shocked the first couple of times I used it, I barely felt the thing graze my skin and it made a nice bleeding hole. It was like witchcraft. Every time I used it I would mentally say, "Cool!"
Design
There are two design points that I want to compliment the FastClix engineers on.
- First, the raised dot where the lancet needle emerges. You can take that little nub and place it against your finger, and by feel, you can have the hole show up exactly where you want it. Sometimes in the past I would try to lance a certain area of my finger and then be surprised to see the blood come out 1/8 inch away from the expected spot. Kind of like drawing on a touch screen device, you can't see what you are doing because your finger is in the way.
- Next, you both cock and fire the device with one pressing motion. It's pretty cool. If you've ever pressed the "go" button on another lancing device and had it just sit there, you know it's annoying to have 2 tasks to complete to get your drop of blood. For instance, if you are driving, stopped at a stop-light, and you test... one extra step is just kind of annoying. I never really thought it was too bad, until I found out that it could be better. It's better.
Sunday, May 20, 2012
Meter madness, jumping to conclusions...
I'm a little excited about the new meter because it came with a lancing device that has been highly reviewed by other glucose checking enthusiasts.
The Fast-clix* lancing device is pretty different. It has a rotating drum of lancets that allow you to change lancets with the flick of a switch, and unload your lancets without exposure to the sharp points. And, you can prick your finger in one easy motion, without "cocking" the device. It is so fancy that I couldn't get it set-up and use it without reading the directions... that's pretty special. After doing this finger poking thing for 25 years or so, you'd think that any device that came your way would be super simple to figure out. Well, this one required just a tiny bit of study.
So here's the creepy bit... (what does this number mean?)
My sensor was reading 170 (post french fry experiment). I Accu-cheked with the new meter and it said I was 240. I was pretty surprised to see such a difference (and, of course my mind went wild wondering if my meter that I use for calibration has been wrong all along, and I've been running 70 points higher for the past couple years).
I tested again, 204. Not good, that's still a decent difference from the CGM and the previous test. I tested again, 213. I took that one as my correction number and delivered a correction.
So, maybe an hour later, after dinner, I test again, 129. That was a fast drop, eh? I still have 2.5 units on board. Did I overdo my correction? I haven't even bolused for dinner yet, maybe I won't. Oh, that's right, when I was over 150 in the late afternoon I turned my basal up, and that's probably what's causing the faster drop. All this with a new meter in my life.
With this new paradigm, I realized that my CGMS sensor is only as good as the meter that calibrates it. I sometimes wonder if my meter is entirely accurate (which we all know, they don't really have to be), and what impact it would have on my overall control to have a legitimately accurate calibration a couple times a day. Just something to think about. It's probably even worth letting integrated devices slip away, if they aren't accurate enough.
Recently, my sister (hi Ariana!) was trying to sort out some glucose mysteries and discovered that her meter was totally erratic and inaccurate. Well, that is not helpful when you are trying to respond to immediate problems... She got a new meter, and I hope that it offers a fresh compass in her quest for good glucose control.
This whole thing brings up a new question... I had been finding that I wasn't feeling any signs of hypo when I got down to 70s and sometimes 60s, when I was using my integrated One-Link meter. Today, I've been at 70-80 (according to my new meter) and I've been noticing my regular symptoms for hypos. It makes me wonder if I've been running higher than I think, all the time... if I calibrate my sensor off of a meter that runs high... and my data is all skewed downward. You wonder more...
My last at-home A1C was 6.7, but, my average blood sugar, according to my sensor had been 133 mg/dl. So, I would expect a 6.3 or so. Maybe my A1C is really telling me that my meter and sensor readings have been bogus to some degree. Maybe I really was averaging 15-20 points higher and never really getting close to hypos, ever. Always something to think about...
The Fast-clix* lancing device is pretty different. It has a rotating drum of lancets that allow you to change lancets with the flick of a switch, and unload your lancets without exposure to the sharp points. And, you can prick your finger in one easy motion, without "cocking" the device. It is so fancy that I couldn't get it set-up and use it without reading the directions... that's pretty special. After doing this finger poking thing for 25 years or so, you'd think that any device that came your way would be super simple to figure out. Well, this one required just a tiny bit of study.
So here's the creepy bit... (what does this number mean?)
My sensor was reading 170 (post french fry experiment). I Accu-cheked with the new meter and it said I was 240. I was pretty surprised to see such a difference (and, of course my mind went wild wondering if my meter that I use for calibration has been wrong all along, and I've been running 70 points higher for the past couple years).
I tested again, 204. Not good, that's still a decent difference from the CGM and the previous test. I tested again, 213. I took that one as my correction number and delivered a correction.
So, maybe an hour later, after dinner, I test again, 129. That was a fast drop, eh? I still have 2.5 units on board. Did I overdo my correction? I haven't even bolused for dinner yet, maybe I won't. Oh, that's right, when I was over 150 in the late afternoon I turned my basal up, and that's probably what's causing the faster drop. All this with a new meter in my life.
With this new paradigm, I realized that my CGMS sensor is only as good as the meter that calibrates it. I sometimes wonder if my meter is entirely accurate (which we all know, they don't really have to be), and what impact it would have on my overall control to have a legitimately accurate calibration a couple times a day. Just something to think about. It's probably even worth letting integrated devices slip away, if they aren't accurate enough.
Recently, my sister (hi Ariana!) was trying to sort out some glucose mysteries and discovered that her meter was totally erratic and inaccurate. Well, that is not helpful when you are trying to respond to immediate problems... She got a new meter, and I hope that it offers a fresh compass in her quest for good glucose control.
This whole thing brings up a new question... I had been finding that I wasn't feeling any signs of hypo when I got down to 70s and sometimes 60s, when I was using my integrated One-Link meter. Today, I've been at 70-80 (according to my new meter) and I've been noticing my regular symptoms for hypos. It makes me wonder if I've been running higher than I think, all the time... if I calibrate my sensor off of a meter that runs high... and my data is all skewed downward. You wonder more...
My last at-home A1C was 6.7, but, my average blood sugar, according to my sensor had been 133 mg/dl. So, I would expect a 6.3 or so. Maybe my A1C is really telling me that my meter and sensor readings have been bogus to some degree. Maybe I really was averaging 15-20 points higher and never really getting close to hypos, ever. Always something to think about...
Saturday, May 19, 2012
Just when you think everything is amost predictable...
Lately I've been reading other d-bloggers talk about their struggles with things like insurance coverage issues and meter accuracy problems. For the last couple years I have been out from under that cloud and pretty content with the material/supplies/equipment side of things. I've been cruising along with my One-Link meter that talks to my pump, and my supplies were being auto-shipped monthly. I was getting 8 strips a day, and normally didn't even need all of them. Then I started using Symilin... and more test strips.
When I ran out before the next shipment arrived I called my doctor to get an Rx for the local pharmacy. Following some phone-tag I had a an order being filled. After I picked it up, I got home and realized that they'd given me Accu-chek strips. Hmmm... must have been a communication problem with nurse at the doctor's office. I went back and asked if they could switch them. Yes, but your insurance doesn't cover One-touch strips here/anymore.
But, that's what works with my pump integrated meter....
It looks like I will have to exclusively get my One-touch strips from Medtronic from now on. And if I need more than 6 strips a day, I will need doctor authorization, etc.
So, what do I do today... with no strips, and no insurance coverage for the ones I use?
First, I thought of buying One-Touch strips with my flexible spending account, which is my own money. Even a small amount of strips to get me through the week would cost me dearly, they run about $1.50/ each these days. After some waffling, I finally decided that the economical move would be to take the free strips (and meter, and lancing device...) from Accu-chek and just input the readings manually until I could get some strips from Medtronic.
So, now I have a new toy. The Accu-chek* Aviva plus, and a Fast-clix* lancing device. I will write about my adventure in adapting to them shortly.
*By the way, what's up with Roche's insistence on spelling their model names so stylistically. I had concentrate to type them "correctly".
When I ran out before the next shipment arrived I called my doctor to get an Rx for the local pharmacy. Following some phone-tag I had a an order being filled. After I picked it up, I got home and realized that they'd given me Accu-chek strips. Hmmm... must have been a communication problem with nurse at the doctor's office. I went back and asked if they could switch them. Yes, but your insurance doesn't cover One-touch strips here/anymore.
But, that's what works with my pump integrated meter....
It looks like I will have to exclusively get my One-touch strips from Medtronic from now on. And if I need more than 6 strips a day, I will need doctor authorization, etc.
So, what do I do today... with no strips, and no insurance coverage for the ones I use?
First, I thought of buying One-Touch strips with my flexible spending account, which is my own money. Even a small amount of strips to get me through the week would cost me dearly, they run about $1.50/ each these days. After some waffling, I finally decided that the economical move would be to take the free strips (and meter, and lancing device...) from Accu-chek and just input the readings manually until I could get some strips from Medtronic.
So, now I have a new toy. The Accu-chek* Aviva plus, and a Fast-clix* lancing device. I will write about my adventure in adapting to them shortly.
*By the way, what's up with Roche's insistence on spelling their model names so stylistically. I had concentrate to type them "correctly".
Saturday, May 12, 2012
weekend basal tinkering, etc.
I've always known that the differences in my weekend sleep schedule should warrant some sort of change to my basal insulin routine, but I never had results that were consistent enough to really work off of. I'm starting to see what I can do differently.
Normally I get up at 5am. In order to counteract dawn phenomenon I have my basal higher by .3 units (approximately) from 2am to 6am. I've been finding that on the weekends if I sleep past 5am, (which I always hope will happen) my blood sugar starts to drop because the DP hasn't gotten rolling as usual, so I'm heading low by 6am.
This AM, for example, I woke up at 5:49AM with an alarm from my CGMS saying that I was 70 mg/dl, but I was really 52 mg/dl. I'm thinking that my solution may be pushing everything forward about 2 hours and seeing if that fixes it. Sleep two hours later, correct DP two hours later? I'll try it tomorrow. (The good news: dropping very slowly and scraping the 50s didn't cause me to have a rebound day.)
Other basal musings:
Also, I think I've become more sensitive to insulin, so I may need to reduce my nighttime basal overall. I've been waking up at the low end of my target range during the past week or so.
I have to say, I sleep really well when I'm in the 70-80 range, when it's stable. Probably because that's close to standard fasting BG for non-diabetics.
Ever since I saw this graph in Think Like a Pancreas, I have wanted to see if I could get as close as possible to the natural basal rate that is observed in human biology. It's fascinating to see that everyone basically has the same rhythms taking place in their system, based on age and time of day. It doesn't seem as much like a guess anymore when you see this average graph. My standard basal rate is fairly close to the dark square plot right now, and it's working for me.
One more thing... it's taken me a couple years to figure out all the features in my pump and CGMS. One of the things I started to use recently is the "silence alerts" feature when I'm sleeping. The alerts that I don't care as much about are the high alerts. If my BG is highish overnight, I normally have already taken the correction and am just waiting for it to take effect. I don't need to be reminded hourly that I'm still out of range. My "high" limit is set fairly low, so it can be annoying to have it tell you when you near or cross the 150 mg/dl line. I have hovered at 150 for hours before and gotten alarms constantly. With "silence alerts" you can silence only the lows or only the highs, or all of the alarms. I find that silencing the "highs" for 7 hours during sleep allows me to only be awakened if I'm having an unexpected low. Carol has appreciated the reduced disruptions to her sleep as well. Even when the pump only vibrates, she is aware of it. Little tweaks like this can offer surprising improvements to your quality of life.
Normally I get up at 5am. In order to counteract dawn phenomenon I have my basal higher by .3 units (approximately) from 2am to 6am. I've been finding that on the weekends if I sleep past 5am, (which I always hope will happen) my blood sugar starts to drop because the DP hasn't gotten rolling as usual, so I'm heading low by 6am.
This AM, for example, I woke up at 5:49AM with an alarm from my CGMS saying that I was 70 mg/dl, but I was really 52 mg/dl. I'm thinking that my solution may be pushing everything forward about 2 hours and seeing if that fixes it. Sleep two hours later, correct DP two hours later? I'll try it tomorrow. (The good news: dropping very slowly and scraping the 50s didn't cause me to have a rebound day.)
Other basal musings:
Also, I think I've become more sensitive to insulin, so I may need to reduce my nighttime basal overall. I've been waking up at the low end of my target range during the past week or so.
I have to say, I sleep really well when I'm in the 70-80 range, when it's stable. Probably because that's close to standard fasting BG for non-diabetics.
| This graph looks so organic and biological, and my basal rate looks clumsy and geometric in comparison... |
One more thing... it's taken me a couple years to figure out all the features in my pump and CGMS. One of the things I started to use recently is the "silence alerts" feature when I'm sleeping. The alerts that I don't care as much about are the high alerts. If my BG is highish overnight, I normally have already taken the correction and am just waiting for it to take effect. I don't need to be reminded hourly that I'm still out of range. My "high" limit is set fairly low, so it can be annoying to have it tell you when you near or cross the 150 mg/dl line. I have hovered at 150 for hours before and gotten alarms constantly. With "silence alerts" you can silence only the lows or only the highs, or all of the alarms. I find that silencing the "highs" for 7 hours during sleep allows me to only be awakened if I'm having an unexpected low. Carol has appreciated the reduced disruptions to her sleep as well. Even when the pump only vibrates, she is aware of it. Little tweaks like this can offer surprising improvements to your quality of life.
Subscribe to:
Comments (Atom)